Remove Data Gaps and FWA within Your Provider Network
Ensure every provider meets credential and eligibility requirements for your government LOBs by ensuring automated data accuracy, completeness and integrity.
Maintain Provider Network Data Integrity
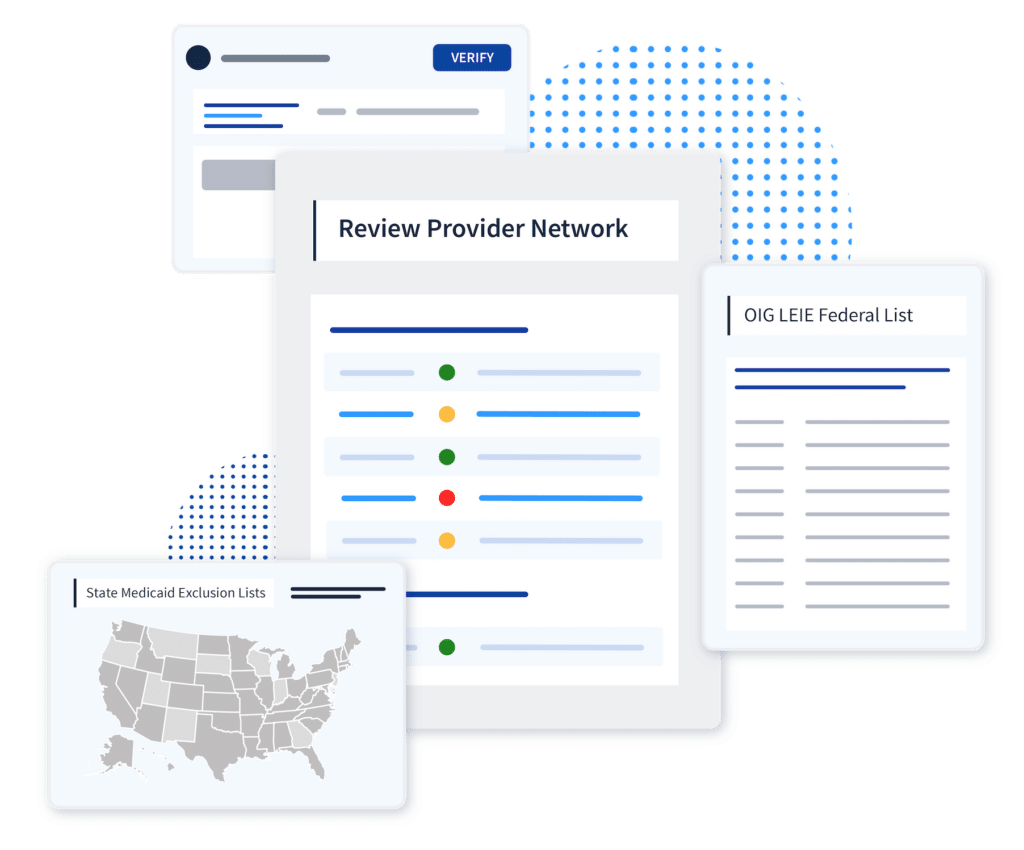
Leverage enriched data to reduce risk and quickly identify fraud
There’s value in peace of mind. We enrich primary source data with unique identifiers to catch and verify issues no one else can. With more robust intelligence at your fingertips, your teams can meet audit and survey requirements with the click of a button.
Complete intelligence on your provider networks
Combine our industry-leading instant license verifications with our OIG, SAM.gov, state Medicaid exclusion monitoring, NPI validation, DEA registration, CMS ordering and referring, Medicare Opt Out, Social Security Death Master File, and more. Customize those requirements by network participation.
Improve Provider Data Accuracy with Verified Credentials
Maintain an up-to-date directory of eligible providers
With continuous monitoring of eligibility requirements, your team can spot provider ineligibility among your network in real-time, providing critical insights for both your par and non-par provider directories.
Defend the integrity of your government LOBs
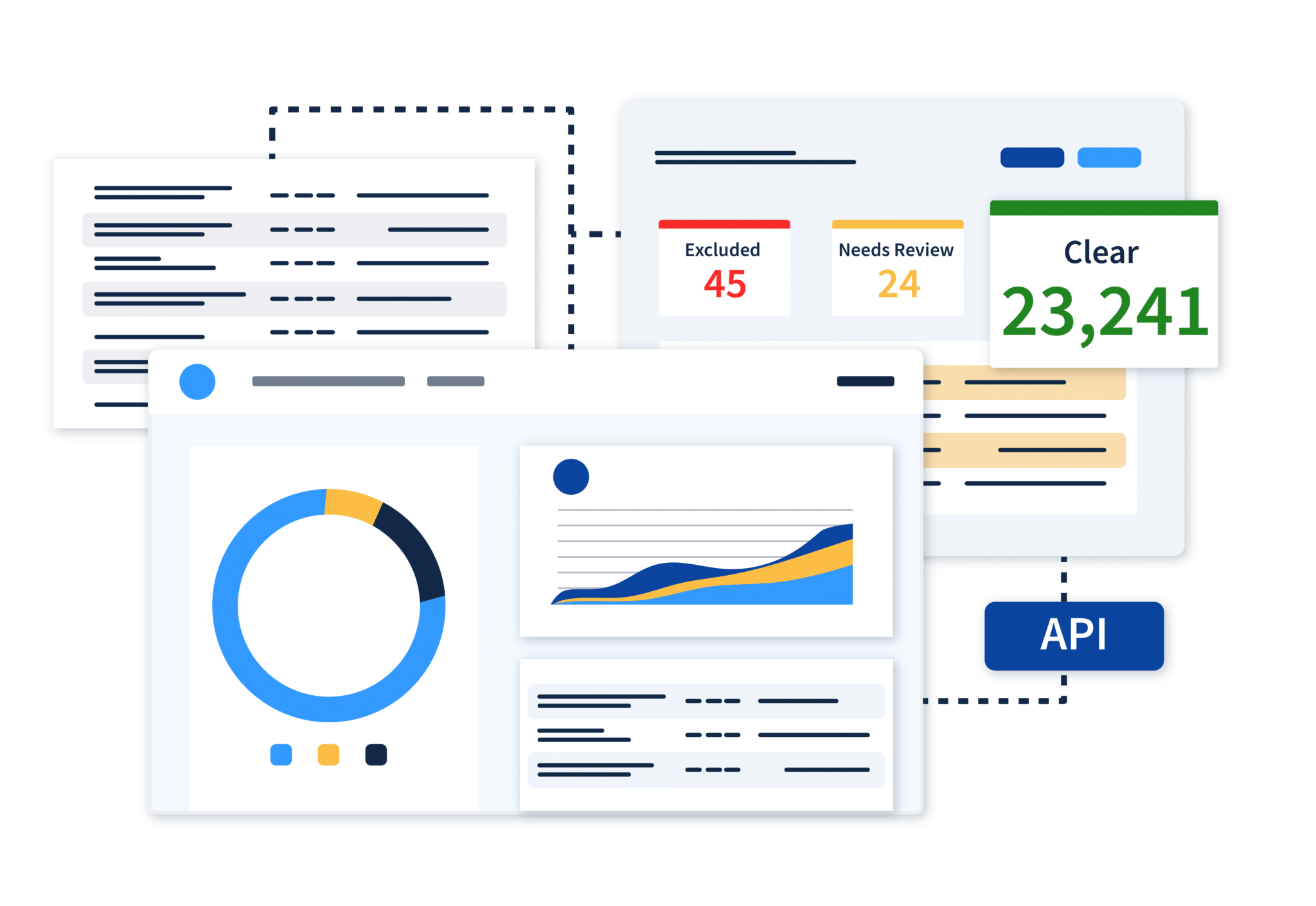
With monitoring that is both smarter and faster, you can catch exclusions and other issues hiding in your provider network among par and non-par providers alike.
Seamlessly Manage Provider Data
Get instant insight and long-term confidence
Credential status changes are delivered directly into existing PDMs or internal data warehouses via API.
Deliver actionable provider network intelligence across your organization
Improve critical processes and break down silos. Our always-accurate provider network data is easily accessible through our software or your system of record. Our flexible integrations empower your teams to make more informed decisions faster.
Data Accuracy and Integrity Built to Scale
Explore our monitoring and verification solutions, especially designed with Credentialing teams in mind.
License and Credential Verifications
Receive the industry’s most accurate automated license and credential verifications directly within your system of record. We deliver results you can trust at exactly the right frequency to prevent eligibility gaps.
API Integrations
Healthcare’s most powerful APIs and integrations for instant compliance verifications across your workflows.
Go beyond regulatory requirements with ease.

Data Security
Ensure SOC II and NCQA-certified security standards and controls.
Network Accuracy
Prioritize patient safety and access beyond initial credentialing.

Reporting and Documentation
Always be audit-ready with primary source documentation for every provider.






