Accurate, Ongoing Compliance Monitoring for Provider Networks
The Industry’s Most Definitive Results
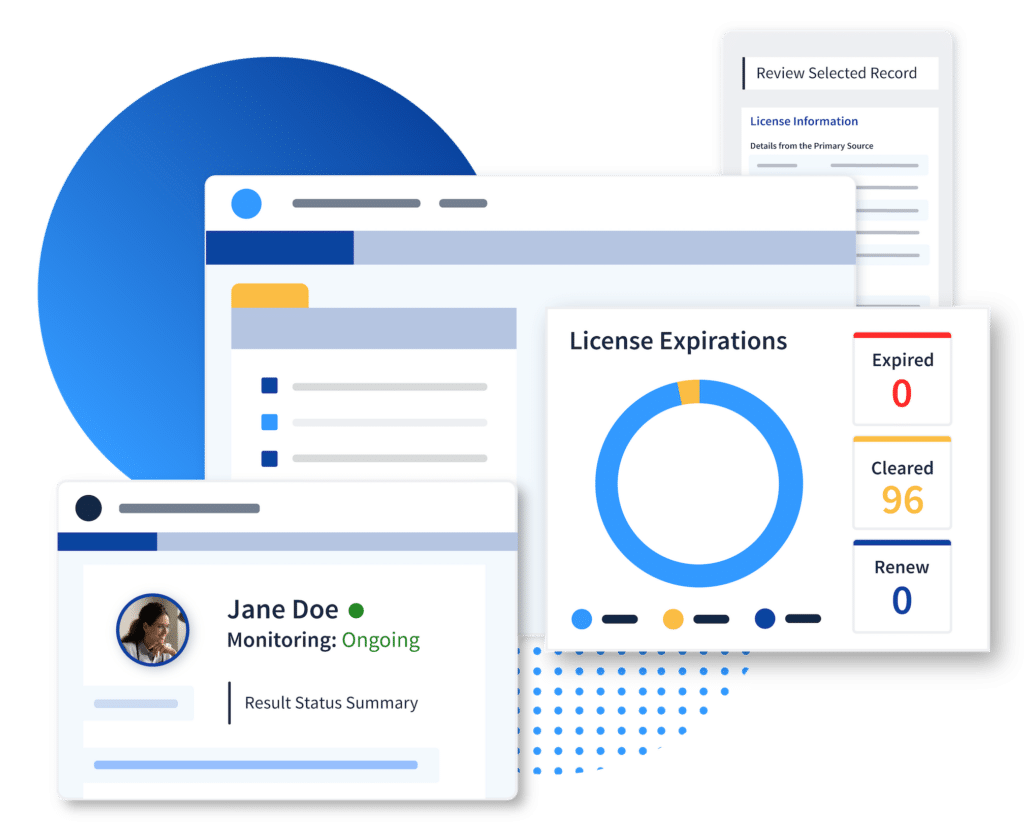
Up-to-Date Provider Eligibility Status
Our HITRUST- and NCQA-certified solution consolidates monitoring processes across par and non-par provider networks and empowers your compliance team with full oversight and audit-ready documentation.
Our proprietary data strategy uses unique identifiers to make our data even better than the primary source, providing exact-match results only with unbeatable accuracy.
Who We Monitor:
- Participating and Non-Participating Provider Networks
- Employees
- Vendors
- First-Tier, Downstream, and Related Entities (FDRs)
- Members
Fully Automated For Continuous Coverage
Ongoing compliance checks for your provider networks
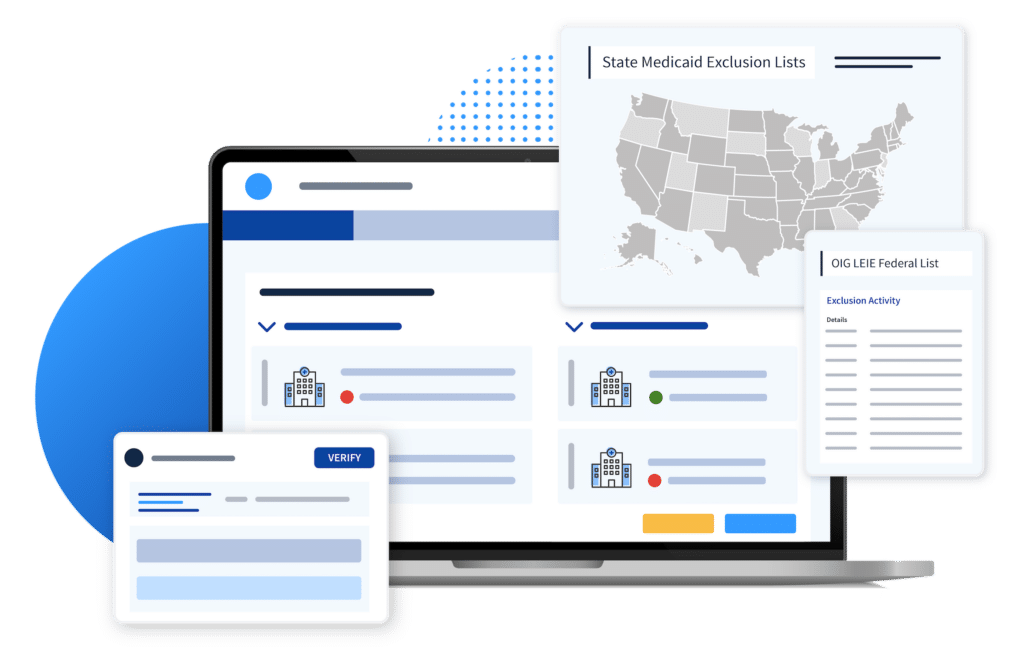
Monitoring for all federal and state exclusion/sanction lists
- HHS-OIG and GSA-SAM.gov
- All State Medicaid Exclusion/Sanction Lists
- CMS Preclusion List
- NPPES NPI Registry
- Medicare Opt Out
- SSN Death Master File
- OFAC SDN and Non-SDN List
- State Licensing Boards
- Specialty Boards
- DEA and/or CDS
NPDB *enterprise clients only


Best-in-Class Data
Exact-match results only
Stay audit-ready with detailed reporting
Organization-Wide Compliance Visibility
Ongoing monitoring for your entire population
Gold-standard vendor data collection and monitoring

Meet DynamicNPI™
Access Verified, Connected Primary Source Data with Just an NPI
DynamicNPI is the payer industry’s most comprehensive source of verified provider data, connecting disparate primary source information directly to NPI numbers.
- Meet credentialing and recredentialing verification requirements in mere seconds
- Speed up time to credential, expediting the path to revenue
- 24/7 access to up-to-date, verified information
- Hands-off NCQA-certified automation you can trust
- Delivered directly within your workflow of choice with ProviderTrust’s turnkey API

“With ProviderTrust, we’ve reduced so much manual work that it has freed up time for our team to focus on additional compliance initiatives that, historically, we just didn’t have enough resources to address. We didn’t have to add staff to get the compliance oversight we always needed.”
Data Integrity Built to Scale
Explore our monitoring and verification solutions, especially designed for Compliance teams.
Provider Credentialing
How an Enterprise Payer Partnered with ProviderTrust for a Compliance Overhaul
Partnering with ProviderTrust allowed the client to automate their exclusion monitoring and primary source verification processes fully.






