According to the U.S. Department of Health and Human Services (HHS), in an effort to eliminate payment to individuals and entities for fraudulent claims, the Office of Inspector General (OIG) reserves the right to exclude individuals and entities from federally-funded healthcare programs for a variety of reasons, including a conviction for Medicare or Medicaid fraud. Those excluded are ineligible for payments from federal healthcare programs for any items or services they furnish, order, or prescribe.
Throughout this post, we’ll look at the HHS’s role in this process, and the different exclusions by way of the Appeals to DAB Administrative Law Judges (ALJ), the Appeals to Board, and the Appeals to the Medicare Appeals Council. Learn how an exclusion monitoring process is essential for mitigating your risk and helping keep patients safe.
What is the HHS Departmental Appeals Board (DAB)?
The Departmental Appeals Board (DAB) provides impartial, independent review of disputed decisions under more than 60 statutory provisions. Previously known as the Grants Appeals Board in 1973 (before a name change in 1980), the DAB’s jurisdiction strictly handled disputes which emerged under the large public assistance grants, such as Medicaid and Aid to Families with Dependent Children, as well as discretionary grant programs.
Throughout the years, the DAB acquired more responsibilities, such as mediating civil monetary penalties (CMPs) and exclusions imposed under a wide range of fraud and abuse authorities (1988), gathering appeals in enforcement cases brought by the Centers for Medicare & Medicaid Services (CMS) (1993), and collecting appeals in Medicare coverage and payment cases and entitlement cases (1995).
According to the U.S. Department of Health and Human Services, the Departmental Appeals Board has the following responsibilities and actions:
DAB Responsibilities
- Three broad areas of jurisdiction, each with its own set of judges and staff.
- A leadership role in implementing Alternative Dispute Resolution (ADR) across the Department since the DAB Chair is the designated Dispute Resolution Specialist under the Administrative Dispute Resolution Act of 1996.
- Staff includes trained mediators and facilitators.
- ADR responsibilities include providing ADR services and training and coordinating and facilitating negotiated rulemaking committees.
DAB Actions
- Resolves disputes with outside parties such as state agencies, Head Start grantees, universities, nursing homes, doctors, and Medicare beneficiaries.
- Generally issues the final say for the Department, but it could be appealed to federal court.
- May issue a recommendation for action by another official.
- Hears disputes that may involve as much as $1 billion in federal grant funds in a single year
Appeals to DAB Administrative Law Judges (ALJ)
The Appeals to DAB Administrative Law Judges (ALJ) scope includes requests from civil monetary penalties and other enforcement actions taken by the Centers for Medicare & Medicaid Services (CMS) against nursing home providers, clinical laboratories, home health care agencies, and other healthcare providers.
The DAB judges determine cases regarding exclusion actions and CMPs imposed by the HHS Office of the Inspector General (HHS OIG) including individuals and other healthcare practitioners, CMPs, as well as the EMTALA or “anti-patient dumping” cases.
ALJs arrange hearings in which the following types of actions are challenged:
- Fraud, abuse, and non-compliance determinations by the HHS IG or CMS.
- Provider/supplier Medicare enrollment and revocation determinations by CMS.
- Terminations of or refusal to grant or continue federal funding for alleged civil rights violations.
- Program Fraud Civil Remedies Act determinations.
- CMP determinations by the Social Security Administration (SSA) by interagency agreement.
- CMP complaints and No Sale Tobacco Orders by CTP by interagency agreement.
- Equal Access to Justice Act determinations relating to HHS IG proceedings.
Appeals to Board
The Board provides a de novo review, which may include an evidentiary hearing of certain types of final decisions of HHS operating components. This means the appeals court may use the trial’s records but reviews the evidence and law without influence from the trial’s former rulings.
Some of the final decisions of HHS operating components include:
- Determinations in discretionary, project grant programs, including disallowances, terminations and denials of refunding, cost allocation plan disapprovals, and rate determinations.
- Determinations in mandatory grant programs, including disallowances of state claims under titles I, IV-A (Temporary Assistance for Needy Families), IV-D (Child Support Enforcement), IV-E (Foster Care and Adoption Assistance), X, XIV, XVI, XIX (Medicaid), and XXI (State Children’s Health Insurance Program) of the Social Security Act.
The Board also provides appellate review of certain types of Administrative Law Judge (ALJ) decisions, which may be appealed by either party. Although, in most cases, the Board decision is the final decision of the HHS.
Appeals to the Medicare Appeals Council
The Social Security Administration (SSA) grants the initial decision on a claim for entitlement to Medicare. A contractor of the Centers for Medicare & Medicaid Services (CMS), including a Medicare Advantage organization, makes the initial determination on an individual claim for Medicare coverage and payment.
If appealed, an Administrative Law Judge (ALJ) grants a hearing. If the parties are dissatisfied with an ALJ decision, a Council review can be requested. The Council may also offer a review of an ALJ decision on its motion. Final Council decisions may be appealed to federal court if the amount in controversy requirements is met.
How to Search DAB Decisions
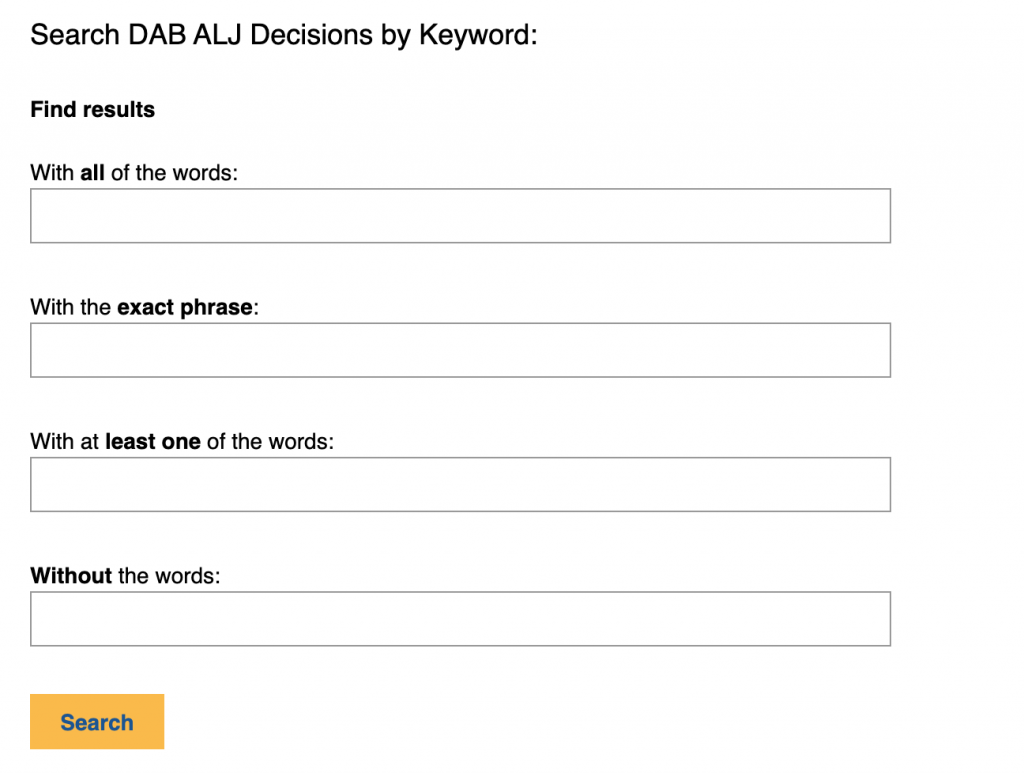
You can easily search DAB ALJ decisions by year since 1985, for CMS, SSA, HHS IG, and FDA actions, including civil money penalties, Medicare enrollment/revocation, and exclusions.
Searching this appeals database can help provide a broader context for why a clinician, organization, vendor, or owner might have become excluded or if they were reinstated.
Exclusion Monitoring for Individuals and Entities
It’s vital to implement and maintain a comprehensive exclusion monitoring approach. According to the OIG, the List of Excluded Individuals and Entities (LEIE) “provides information to the healthcare industry, patients and the public regarding individuals and entities currently excluded from participation in Medicare, Medicaid, and all other federal healthcare programs.” If you’re going to hire a new employee or work with a new vendor, you need to know their background. That’s your cue to check the OIG’s List of Excluded Individuals and Entities (LEIE).
A healthcare law firm (Arnall Golden Gregory LLP) described how two recent DAB appeal decisions support the importance of regular background screenings and exclusion checks for all employees and managing individuals. Remember to do your homework before working with the individual or entity. If you hire someone on the list, you may be subject to civil monetary penalties.
To avoid liability, routine monitoring is always advised. With CMS and HHS OIG working harder than ever to eliminate fraud in Medicare, Medicare, and others, you will be held accountable for your relationships with excluded individuals and entities.







