When it comes to measuring healthcare license monitoring and identifying how it applies to various organizations, HR professionals, and overall compliance – the reactions and responses can be quite different. Due to unique company policies, procedures, and systems, there is a lack of uniformity amongst the healthcare community related to this vital piece of the credentialing process.
Government regulations and accreditation requirements leave quite a bit of ambiguity, confusion, and interpretation regarding creating a gold standard for ongoing provider license monitoring. Whether you have years of experience or are recently exploring the opportunities and constraints of license verification and continuous provider monitoring, it is essential to understand how to optimize your strategy and reduce your risk. In this post, we will explain some of the best practices to help you grow and succeed.
Healthcare License Authorities
It’s important to understand the complexity of healthcare credentialing and license verification according to each authority that is involved in determining who is eligible to provide quality care. To do this, let’s review the authority figures as they relate to the rules and requirements for each licensed provider and healthcare organization.
National Healthcare Certification and Registration
National certification and registration organizations exist to verify that each individual has completed the proper requirements for their specific job title or discipline. A prominent example would be American Allied Health which provides online certification for a variety of positions including many technicians or medical assistant roles. Providers can register and obtain a national certification once they have supplied proof of educational and experience requirements, and passed an exam.
State Board of Medical Examiners
Each state has a State Board of Medical Examiners, which is responsible for administering healthcare licenses to qualified candidates who have graduated from approved medical schools and who have completed appropriate educational requirements. According to provider discipline or specialty, each individual is required to hold a valid license or certification from a state board authority to administer care.
State boards of medical examiners help safeguard the health, safety, and welfare of each patient in their state and are responsible for investigating and providing disciplinary actions to licensees who are found guilty of violating specific state Medical Practice Acts.
Many state health professional medical boards provide administrative support to the boards, committees, councils, and registries that are responsible for licensure and regulation of their respective healthcare professionals.
Joint Commission and Healthcare Accreditation License Standards
Healthcare accreditors are non-profits who partner with a variety of healthcare organizations to promote and evaluate quality standards and safety requirements that impact care. The Joint Commission, NCQA, URAC, CARF, and more help ensure that healthcare providers are delivering safe and valuable patient care.
The expectation is that licensed employees must be able to account for their credentials once a survey takes place to maintain the healthcare organization’s respected accreditation. Because surveys are unannounced, each healthcare organization must have effective licensure, certification, and registration processes that deliver real-time results, up to a daily evaluation or verification.
HHS OIG and CMS Guidelines
HHS Office of Inspector General has the authority to impose fines and penalties for inadequate credentials or false claims billed. If the individual associated with inadequate licensure or credentials is part of a bundled care service, you will reimburse Medicare/Medicaid for a percentage of wages paid, depending on your agreement with the state. If the individual associated with inadequate licensure or credentials is billing Medicare/Medicaid directly for a specific service this could be considered an overpayment. Therefore, your organization may be responsible for repaying the reimbursement received for the services performed or care given.
How Often Should I Verify Healthcare Licenses?
Healthcare organizations should be confident that the frequency at which they are verifying licenses, certifications, and registrations is sufficient to ensure that no individual is providing services without a renewal lapse or administrative action against their license at the time of care.
Keeping up with so many licensed provider credentials across your healthcare organization can be extremely difficult. Traditionally, it is accepted that healthcare license verification occurs upon hire and time of renewal, and the common standard that HR professionals are held accountable. However, as you can imagine, this baseline standard two-touch approach can leave some critical gaps or blind spots in your assurance of properly credentialed providers.
Whether you find yourself managing this process at a large organization or individual facility, developing and implementing an ongoing solution is critical to comply with each state licensure board, Joint Commission and accreditation standards, CMS and OIG Guidelines, and internal policies. Having a system in place with the ability to monitor and verify licenses at multiple frequencies (up to daily) enables you to feel confident that you are not missing any license status changes or sanctions against providers as they continue to supply care.
Healthcare License Monitoring Best Practices
Understand Your Provider and Employee Populations
Starting with a roadmap for the types of licenses, certifications, and registrations you will need to monitor is key to running a successful monitoring program for employees and providers. Because every healthcare organization is unique, there will be a variety of databases and registries that are relevant for your populations for each discipline and/or job responsibility.
Understanding the scope of work required for accurate and timely credential verification from primary sources helps you evaluate your resources and optimize your process and team contributions. Due to the complexity of aggregating data from so many sources, many healthcare organizations choose to partner with a third-party vendor for effective healthcare license monitoring. Partnering with a healthcare data expert helps minimize risk, saves you time, and provides a means to stay on top of provider information and credential renewals.
Establish a Consistent Credentialing Process
How are you managing your current credentialing process as it relates to verification, privileging, screening your providers, and more? Do you have consistent and clear guidelines company-wide for your credentialing policies and procedures? Our team has found that healthcare Human Resource professionals have significant challenges regarding putting their credentialing policies and procedures into action.
Think about the difficulty of holding every facility, department, and team member accountable to follow oversight for each licensed or certified provider. We’ve found that the most successful leaders have clarity around the procedures that need to be followed and a core set of guidelines for expectations and implementation.
Many organizations do not have a centralized system for submitting, analyzing, syncing, and automating data processes for each provider to ensure license renewals and disciplinary actions don’t go unnoticed. HR and Compliance professionals are working in and out of many programs each day (HRIS, ATS, etc.) and need a reliable and efficient data flow to help support their daily tasks and employee management.
Leaders must have the ability to remove communication barriers and supply an environment for quick action and trust between all contributors in the credentialing, verification, and renewal process.
Communicate License Monitoring Requirements
When it comes to properly credentialing each licensed provider, how aware is your team of potential risks related to fraudulent activity or inefficient government reporting? With high demand and a short supply of nurses and other critical roles, it’s important to uphold quality and compliance standards when sifting through many candidates and credentials. Has your team set priorities for each component of the verification process, and established the right checks and balances to be confident in your hiring process?
Because there are so many accrediting bodies and state board authorities to monitor, it is crucial to understand the healthcare licensure requirements for each job type and specific provider role. Thankfully, data support and license monitoring solutions for healthcare Human Resource professionals are more readily available to fill the gaps in accessing, referencing, and complementing provider profiles and credentials from thousands of databases, registries, or offline documents.
To build a comprehensive approach to license monitoring, finding the right balance between automated tools, excellent communication, and industry knowledge will help ensure a transparent and consistent workflow.
Optimize Your Primary Source Verification
What’s your first thought when considering primary source verification? Are you stressed, confused, or overwhelmed? How are you currently validating and tracking so many credentials and knowing which sources to check? Even if you know where to get the information, do you have a platform or tool to help automate some of the small details? Our team believes that many healthcare professionals are bogged down with excessive administrative work, and tedious tasks that add up, taking time and resources away from their primary focus – developing the people who deliver care.
Do you utilize the services of a Credential Verification Organization (CVO)? Does your organization rely on an internal process using spreadsheets or manual searches? We’ve been partnering with many healthcare organizations over the years to determine their pain points with license verification and ongoing monitoring. We’ve created a smarter monitoring solution where teams can feel confident and comfortable that their primary source verification is optimized to support informed decision-making.
Provide Feedback Loops Between Human Resources and Compliance
Let’s face it, sometimes interdepartmental collaboration between Compliance and Human Resources can feel a little disjointed. While some team members may be focusing on finding certain needles in a haystack, others are just trying to keep their heads above water by filling positions and trying their best to keep their staff happy. Open communication between these departments is critical to ensuring the right people are delivering care.
Feedback loops help both departments set more actionable and measurable goals that can lead directly to reducing risk and improve the efficiency of credentialing. Traditionally, these two departments face structural challenges related to integrating systems and processes that intersect with provider credentialing, monitoring, and personal development.
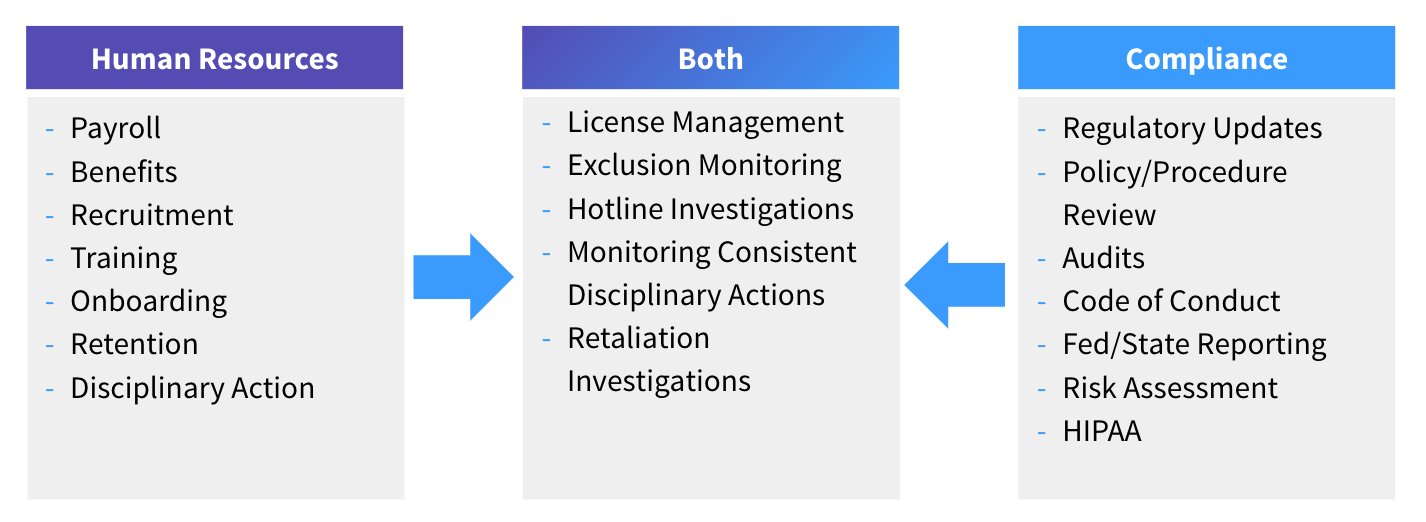
We’re proud to bring both audiences together by offering a way for easy dialogue with automated tools and a platform built for documenting, tracking, and providing timely alerts for daily compliance and continued success. ProviderTrust firmly believes that when these groups can work together, it provides smarter and safer healthcare for everyone.







