In 2006, New York’s Office of the Medicaid Inspector General (OMIG) was established as an independent office within New York State’s Department of Health to combat fraud and abuse in New York State’s Medicaid program.
The OMIG’s mission is “to enhance the integrity of the New York State Medicaid program by preventing and detecting fraudulent, abusive, and wasteful practices within the Medicaid program and recovering improperly expended Medicaid funds while promoting a high quality of patient care.”
To carry out this mission, the OMIG coordinates the detection, investigation, audit, and review of Medicaid providers and recipients to ensure they comply with state and federal laws and regulations. Though the OMIG is an autonomous, independent entity that serves to protect the integrity of New York’s Medicaid program, it works closely with many offices, including:
- Centers for Medicare and Medicaid Services (CMS)
- The Office of Inspector General (OIG)
- New York State Attorney General’s Medicaid Fraud Control Unit (MFCU)
- The Bureau of Narcotic Enforcement (BNE)
- Law enforcement and other state agencies
The OMIG reports to the Governor, but it has the authority to pursue both civil and administrative enforcement actions against individuals and entities that engage in fraud, abuse, and other illegal practices.
What is New York's OMIG List of Restricted and Excluded Providers?
The OMIG List of Restricted and Excluded Providers is New York State’s exclusion list. Updated daily, this list identifies individuals and entities that have been excluded from participating in the State’s Medicaid program, of which there are about 8,000. There are many reasons an individual or entity may be excluded, but the OMIG is primarily concerned with the fraud, waste, and abuse of Medicaid services by providers and Medicare patients and members.
Provider fraud includes:
- Billing for Medicaid services that were not provided
- Billing for unnecessary services
- Selling prescriptions
- Intentionally billing for a more expensive treatment than was provided
- Giving money or gifts to patients in return for agreeing to get medical care
- Accepting kickbacks for patient referrals
Patient/member fraud includes:
- Lending or sharing a Medicaid Identification card
- Forging or altering a prescription or fiscal order
- Using multiple Medicaid ID cards
- Re-selling items provided by the Medicaid program
- Selling or trading the card or number for money, gifts, or non-Medicaid services
Once an individual or entity has been excluded, OMIG will automatically suspend them from participating in the Medicaid program. No payments will be for medical care, services and supplies furnished, prescribed, or ordered by an excluded party. An excluded person also cannot be involved in any activity related to furnishing medical care to recipients who intend to submit claims to the State Medicaid program. In addition, excluded providers reimbursed on either a cost-related or a fee-for-services basis may not submit any claims or be reimbursed for any medical care or services if they are found in violation of any kind of state or federal regulation.
Who needs to monitor the OMIG List?
If your organization participates in federal healthcare programs (Medicare, Medicaid, CHIP, VA), either by directly furnishing goods or services or indirectly, but working with a healthcare provider, then you need to monitor the OMIG List of Restricted and Excluded Providers.
Screening your healthcare populations against Medicaid exclusions is not only one of the most valuable defenses in protecting your organization and patients, but they also ensure the integrity of healthcare dollars. To ensure that healthcare employees are not on any exclusion lists, Medicaid providers must regularly screen all of their employees (from pre-employment and on an ongoing basis).
Organizations that employ or conduct business with an excluded provider may be subject to Civil Monetary Penalties (CMPs). CMPs enforced by HHS OIG or false claim allegations by the U.S. Department of Justice (DOJ) can result in more than $20,000 per false claim or statement, plus treble damages. Here are the latest CMPs published by the OIG.
How do I check the NY OMIG List of Restricted and Excluded Providers?
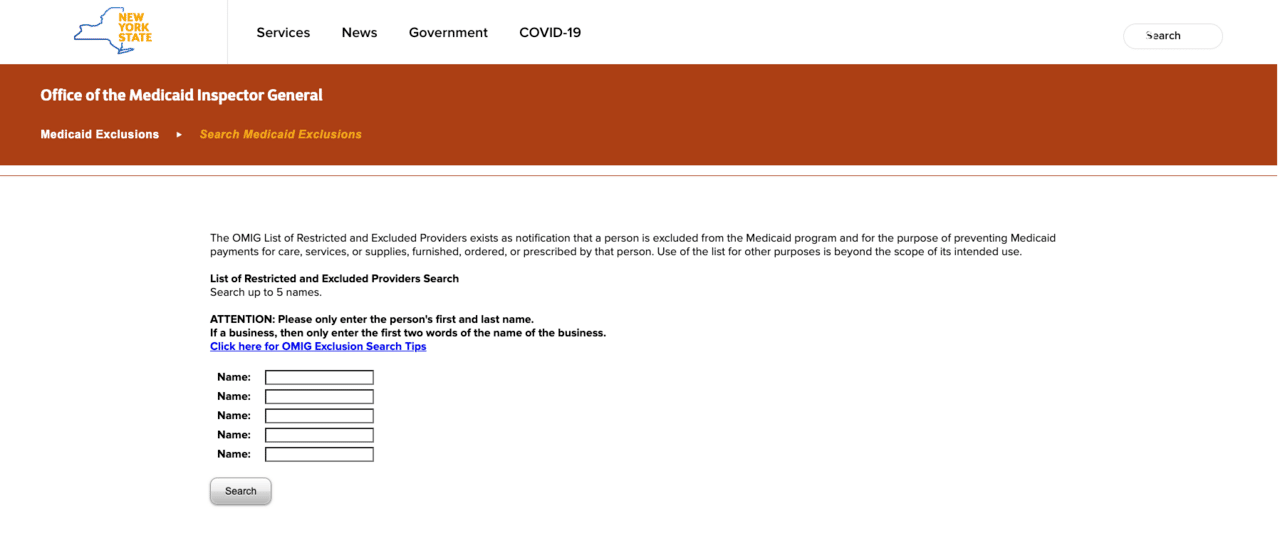
OMIG offers two options for searching the State Exclusion List. The first is a web-based search function that allows users to search up to five names at a time. The second option offers multiple downloadable formats that offer full access to the exclusion list. The list is available as a formatted list, a tab-delimited list for exporting into applications or desktop spreadsheets, an excel spreadsheet, or a short list showing exclusions commenced within the last 30 days.
Identifying Matches on the OMIG List of Restricted and Excluded Providers
Data Completeness
As far as the numbers go, you might wonder how complete the OMIG List of Restricted and Excluded Providers is. Here are our findings:
- 0% have addresses, city, or state information
- 73% have a license number
- 24% have a National Provider Identifier (NPI)
- 0% have SSN or DOB
Because high-confidence, high-quality exclusion matches are only possible by matching uniquely identifying data (such as an SSN or NPI), it can be difficult and time-consuming to confirm New York exclusions manually and catch bad actors who may be using a different name or license.
NY OMIG List of Restricted and Excluded Providers FAQ
We suggest capturing the provider’s SSN so you can use the SSN verification tool. If you don’t have an SSN but have the provider’s DOB, you might be able to conduct a successful search. The same goes for connecting a license and a DOB.
Also, it should be noted that you can enter incomplete information into any search criteria. Examples include having the birth year only instead of the complete DOB and adding the first few letters of the provider’s name.







