Every year, the Department of Health and Human Services (HHS) and the Office of Inspector General (OIG) publish a summary of the Top Management and Performance Challenges Facing HHS. This report helps HHS fulfill its mission to improve the health and well-being of Americans while also providing suggestions for how healthcare organizations can stay ahead of the curve to avoid and combat fraud, waste, and abuse.
Though HHS has made efforts to address the challenges outlined in this year’s report, there are still many opportunities for improvement in 2024. We’ve broken down the report’s primary themes and how they affect healthcare organizations moving forward in 2024.
Ensuring the Financial Integrity of HHS Programs
In fiscal year (FY) 2022, improper payments within healthcare programs like Medicare, Medicaid, and Children’s Health Insurance Program (CHIP) were estimated at a staggering $131.6 billion. These improper payments encompass a variety of discrepancies, ranging from duplicate payments and funding services that don’t meet eligibility criteria to extending coverage to ineligible recipients, paying ineligible providers, and other program guideline violations.
Despite the Centers for Medicare and Medicaid Services (CMS) efforts to target long-standing problematic areas (such as hospice, home health, hospital outpatient, and skilled nursing facility care), the battle against improper payments within Medicare fee-for-service programs remains challenging. New concerns have also surfaced—unusually high-billing labs, upcoded hospital stays to inflate reimbursements, and issues related to genetic testing will require close attention going forward.
With Medicaid, the challenges are equally formidable. HHS estimated that over 15% of payments in FY 2022 were improper. In addition, the COVID-19 public health emergency triggered shifts in Medicaid and CHIP eligibility, which could impact millions of people. Medicaid enrollment and renewal processes for all states must adhere to Federal statutory and regulatory requirements, and CMS is responsible for ensuring these programs continue to serve and maintain coverage for eligible beneficiaries.
HHS also disperses taxpayer funds through grants and contracts, and it must provide clear guidance and up-to-date policies on financial management, internal controls, and compliance with regulations. Oversight is crucial to ensure the grant’s sub-recipients utilize these funds appropriately and for their intended purpose. HHS must identify, remedy, and prevent instances of fraud, waste, and abuse to ensure taxpayer money is not used for inappropriate, unauthorized, or illegal purposes.
HHS’s suspension and debarment programs are vital to upholding integrity in Federal grants and contracts. These programs ensure that the government engages only with law-abiding individuals and uses taxpayer dollars appropriately. They have enhanced their programs through outreach, training, and guidance, but opportunities for improvement still exist.
HHS will continue its efforts to ensure fiscal responsibility and regulatory adherence across all Medicare and Medicaid programs and funding mechanisms. They will work to improve contract management and closeout processes, stay vigilant of embezzlement, theft, and novel fraud schemes, and prevent future occurrences of improper payments.
Improving outcomes in Medicare and Medicaid
Safeguarding the integrity of Medicare and Medicaid programs is vital to ensuring they deliver quality care to enrollees and high value to taxpayers. HHS-OIG has outlined its intention to focus on fraud prevention, detection, and enforcement to recover inappropriately allocated funds, protect patient wellbeing, and hold bad actors accountable.
While remaining vigilant of abuse is important across all types of healthcare organizations and provider types, it is especially vital in high-risk industries and areas, including:
- COVID-19 test billing
- Durable medical equipment
- Home Health
- Hospice
- Genetic testing
- Medical identity theft
- Treatment for substance use disorder
Each of these areas presents one-of-a-kind challenges and vulnerabilities that will require keen oversight.
CMS programs such as managed care, traditional Medicare, or various value-based care models take on different risks due to their unique payment and coverage structure. As HHS evolves to revise payment policies and incentives, it must anticipate that these payment designs will be exploited. Proactive measures are more important than ever to address vulnerabilities and stay aware of potential avenues for fraud, waste, and abuse, especially as managed care continues to expand. Managed care now covers more than half of Medicare enrollees and over 80% of Medicaid enrollees.
Unfortunately, Medicare Advantage programs are not exempt from instances of fraud, waste, and abuse. Bad actors within these organizations claim additional government payments using a number of schemes. This includes overemphasizing the sickness of their patients and avoiding costs by denying care that would be covered by Medicare. CMS must bolster its oversight mechanisms—specifically honing in on chart reviews and health risk assessments conducted by plans—to ensure risk-adjusted payments accurately reflect an enrollee’s health status.
CMS also plans to improve its managed care oversight by reducing inappropriate prior authorization and payment denials that put plan profits above enrollees’ well-being. CMS has recently taken measures to improve the information that enrollees can access about Medicare Advantage prior authorization and coverage decisions. Ongoing updates to the risk adjustment model aim to improve accuracy within Medicare Advantage.
Protecting HHS Beneficiaries
Federal healthcare programs are responsible for delivering safe, high-quality care that patients and beneficiaries can obtain without encountering needless burdens or disparities. Though HHS continues to work towards bettering these programs, there is still much to be done to improve access to and quality of care. Unfortunately, patient harm is still very much part of the healthcare landscape.
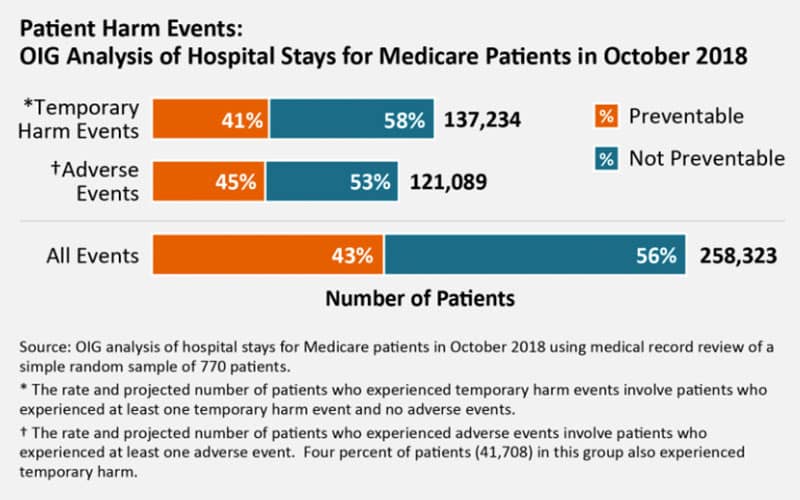
The report includes the following chart analyzing known patient harm events:
HHS must work diligently to ensure patient safety and protection. Many providers earn their patients’ trust and work hard to deliver exceptional healthcare services, but still, a population of providers harms people.
Conducting background checks for providers and staff is vital to preventing potential predators from working for federal programs. Comprehensive vetting should also occur in childcare programs, nursing homes, and HHS-funded healthcare settings, though it’s important to remember that patient abuse can occur in any care environment.
Reporting abuse cases can be challenging, particularly in non-facility settings like home-based services or group residences. All states have laws mandating that professionals ranging from doctors and nurses to elementary school teachers report suspected abuse. However, more support is needed for victims, and holding perpetrators accountable is extremely important.
States can better detect unreported abuse and neglect cases by leveraging claims data. A 2019 HHS-OIG guide outlines a catalog of diagnosis codes indicating potential abuse or neglect, conducts regular data assessments, and promotes the use of data to aid compliance with reporting laws. CMS must guarantee that its reporting standards safeguard individuals across all healthcare environments. Shielding patients from abuse and neglect is a primary mission for CMS that demands the focus and collaboration of all stakeholders.







